Anthrax
|
Bacillus anthrachis causes Anthrax |
Local names: Luo: Aremo / Embu: thita / Kamba: ndulu / Gabbra: chimale, chirrmalle / Kikuyu: Muriru / Kipsigis: bursta / Nandi: purasta / Maasai: Emburwo, ol akirikir, ol ogereger, em bjangat, eng eanairogua / Maragoli:likenji / Samburu: lokuchum, nokulupo / Somali: kut, khut, kud, baargariirshe / Swahili: kimeta, imetha / Turkana: enomokere, lolewe, lookot, lotorob, lokuchum / Iteso: atular / Luidakho: lishenji / Luvugusu: muyaka / Common names: fievre charbonneuse, charbon (French) carbunco bacteridiano (Spanish) Description: Zoonotic disease Hosts: Anthrax is a soil-borne bacterial infection of domestic animals, wild animals and human |
||||||
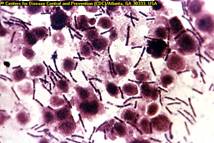
| © Center for disease control (CDC) Atlanta, Georgia | |||||||
Introduction
| WARNING: Notifiable disease! If you suspect an animal has anthrax, you must inform the authorities immediately. Animals suspected of having died of anthrax should not be opened. |
Anthrax is a soil-borne bacterial infection of domestic animals, wild animals and human. It is caused by the spore-forming organism Bacillus anthracis.
Hosts: It is most common in wild and domestic herbivores – cattle, sheep, goats, camels, horse, pig, dog, antelopes, zebra – but it also occurs in humans exposed to tissue from infected animals, contaminated animal products, or directly to anthrax spores. It doesn't affect chickens but it is common in ostriches.
Distribution: Anthrax occurs all over the world. It is more common in warm climates as spore formation only occurs when the temperature is between 20˚ and 40˚C, the humidity is over 60% and the pH is above 6.0.
Under such conditions spore formation occurs rapidly, leading to the contamination of soil and water, where the spore may survive for years; up to 30 years in some cases. Spores are formed in the presence of oxygen. Within a carcass the organisms rapidly die. Only when they are exposed to air and oxygen do they form spores.
Mode of spread
The disease is transmitted through pastures which are contaminated by the spores. The animals may be forced during drought to graze on short grass which may be contaminated by the infected soil. Anthrax spores can remain infective in soil for many years. During this time they are a potential source of infection to grazing livestock. Grazing animals may become infected when they ingest sufficient numbers of these spores from the soil.
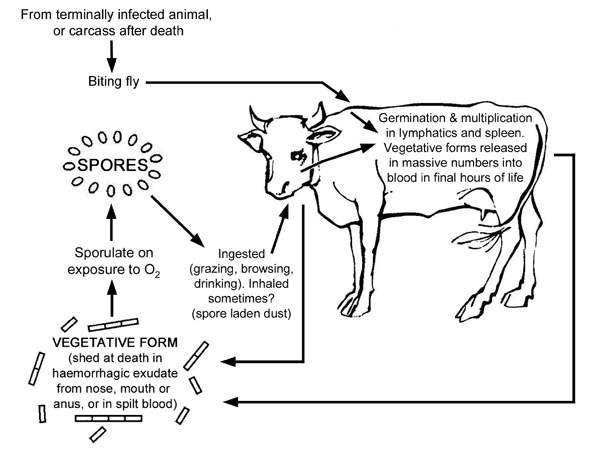 |
|
Anthrax cycle of infection, amended from Anthrax Guidelines WHO |
|
© CABI: Animal Health and Production Compendium, 2007 Edition.
|
- Feed contaminated with bone, or other meal from infected animals, can serve as a source of infection for livestock, as can hay that is heavily contaminated with infected soil.
- Infection is influenced by communal watering points. Water holes used by different species of animals are known to be a source of infection.
- Flooding may expose previously buried spores and agricultural practices may do the same.
- Tissues of infected animals may be moved by rats and carrion eaters and transfer infection.
- Raw or poorly cooked contaminated meat is a source of infection for carnivores and omnivores, including humans.
- In animals, infection is usually by eating infected grass, less commonly by breathing spore infested dust or through open wounds. In cattle, sheep and goats infection is nearly always by mouth.
- In camels and horses biting flies may transmit infection and this may explain the swellings sometimes seen on the body and legs of these species.
- Humans are fairly resistant and are infected after an occupational hazard affecting workers in tanneries. The workers may inhale spores and suffer an acute fatal pneumonic form of anthrax. Cutaneous anthrax is common among people who carry meat and other animal products from infected carcass. The bacteria can survive for several years in livestock products such as hides, wool and bones.
- Infection in humans is usually via skin abrasions or by inhalation. People handling wool, hides and skins are mostly at risk. Eating infected meat obviously carries a major risk, although rapid cooking quickly destroys the organism before the highly resistant spores have a chance to develop. There has been cases reported in Kenya where people have eaten meat from infected animals and died shortly afterwards.
 |
|
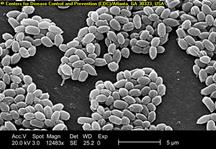
Spores of Anthrax can survive for many years © CDC Atlanta, Georgia
|
Signs of Anthrax
Depending on the route of infection, host factors, and potentially strain specific factors, anthrax can have several different clinical presentations.
The anthrax bacillus produces a lethal toxin in the animals which causes accumulation of fluid (oedema=swellings) and tissue damage, resulting in death from shock and kidney failure.
In very severe forms, there is a short illness and this makes the disease difficult to treat. The animal develops high fever, difficult breathing followed by convulsion, collapse and death.
In ruminants such as cattle, sheep and goats, the symptoms of anthrax are very sudden and severe, with death occurring within minutes to hours. There is staggering, high fever, rapid breathing, trembling, collapse, and a few convulsive movements, followed by death. Usually the animal is found dead, with bloody discharges from body openings. Rigor mortis is often absent or incomplete, with marked bloating and rapid decomposition. The blood is dark and thickened and fails to clot readily. If by mistake the carcase is opened it will be noticed that the spleen is greatly enlarged and the pulp soft and tarry.
In severe forms, the disease would last about 2 - 3 days before death. The animal will appear depressed, listless and have high fever. The mucus membranes in the eyes and gums are congested and hemorrhagic(showing blood). There is difficulty in breathing caused by edematous (watery) swelling in the throat.
In less severe cases, some animals may survive for 1 week and others will recover. In dogs, humans, horses and pigs, the disease is usually less severe. Sometimes there may be swelling in the lower neck, chest and shoulders, especially in animals such as pigs, camels and horses.
In both severe and less severe cases, affected cows may abort and have a reduction in milk production. The milk will be blood stained or appear yellowish in color. Infection in the alimentary tract may cause dysentery.
Diagnosis
In any case of sudden death anthrax must be suspected and a veterinarian informed so that a diagnosis can be made. Bloat, lightning strike, blackquarter, snakebite, and plant poisoning can also cause sudden death.
It is very risky for unqualified laboratory personnel to take samples of the disease. The sampling procedure should be carried out by qualified laboratory personnel only.
Blood from nose, mouth or anus is a tell-tale sign of Anthrax. It may be a lot or a few drops. It can also be absent.
The vet will stain a blood smear or smear from a lymph node, abdominal fluid or subcutaneous sweling and examine it under the microscope to give a rapid diagnosis. Only if the result is negative should the post mortem examination proceed. Under the microscope the organism appear as large square ended rods with a pink capsule.
 |
|
Deceased zebra with signs of Anthrax |
|
© Peter C B Turnbull
|
Prevention and Control
Prevention and control requires a strict adherence to veterinary regulations to prevent and minimize the spread of the disease among livestock and humans.
Anthrax can be a very severe food borne pathogen and must at all means be prevented from entering any food or feed.
- The carcass of any animal suspected to have died of Anthrax should not be opened but must instead be burnt or buried at a depth of at least 2 meters, and the surrounding area burnt and treated with 10% formalin or 10% caustic soda to prevent contamination of the environment. The surrounding area where the carcass has been burned should be fenced off.
Signs after death
- Carcass is stiff and bloated
- Decomposition is rapid
- Bleeding from ears, mouth, nose, anus or vagina
- Blood is dark and does not clot
 |
| Suspected anthrax case: A deceased pig with signs of Anthrax is enclosed in a plastic bag to prevent loss of body fluids before a smear of fluid from an appropriate site is taken |
|
© John Walton (deceased)
|
Contaminated beddings, premises and feeds should be destroyed or thoroughly disinfected.
- Vaccination of all livestock at risk should be done annually as a legal requirement. The avirulent live Sterne- strain spore vaccine, which has lost its ability to form capsules, is available in most countries and offers annual protection. In Kenya a commercially available product called “Blanthax” is used for the annual vaccinations against Black quarter and Anthrax.
- Quarantine should be imposed in all infected areas to prevent movement of animals into and out of such areas. Such quarantine should be not lifted until at least 6 months after disinfection procedures are complete.
- The appropriate authorities must be notified.
- General sanitary measures must be observed by all persons handling diseased animals, both for their own safety and to prevent spread of the disease.
- Scavengers, including dogs, jackals and birds, must be controlled and kept away from dead animals to minimise spread of infection.
- Remove healthy animals from the vicinity where an animal has died.
Recommended treatment
Bacillus anthracis is susceptible to antibiotics such as penicillin, streptomycin and tetracyclines and these may be used by a qualified veterinarian either to treat infected animals in the unlikely event that they are seen alive, or to give protection to in-contact animals. This is then followed by vaccination about 7-10 days later.